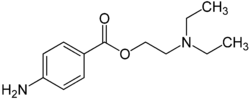
Procaine ( novocaine , diethylaminoethyl ether p- aminobenzoic acid hydrochloride ) is an anesthetic with moderate activity.
| Procaine | |
|---|---|
 | |
 | |
| Chemical compound | |
| IUPAC | 2- (diethylamino) ethyl 4-aminobenzoate |
| Gross formula | C 13 H 20 N 2 O 2 |
| Molar mass | 236.31 g / mol |
| Cas | |
| PubChem | |
| Drugbank | |
| Classification | |
| ATX | |
| Pharmacokinetics | |
| The half-life. | 40–87 seconds |
| Dosage Forms | |
| Powder for solution preparation, injection solution (2.5%, 5%), ointment for external use, rectal suppositories | |
| Route of administration | |
| parenteral | |
| Other names | |
| Novocaine | |
Included in the list of vital and essential drugs .
Content
History
Novocaine was first synthesized in 1898 by the German chemist Alfred Einhorn as a replacement for cocaine used at that time for local anesthesia.
Pharmacological action
A local anesthetic with moderate anesthetic activity and a wide range of therapeutic effects. Being a weak base , it blocks Na + channels, prevents the generation of impulses at the ends of sensory nerves and the conduction of impulses along nerve fibers. Changes the action potential in the membranes of nerve cells without a pronounced effect on the resting potential. Suppresses the conduct of not only pain, but also impulses of another modality. When absorbed and directly introduced into the blood stream , it decreases the excitability of peripheral cholinergic systems, reduces the formation and release of acetylcholine from the preganglionic endings (has some ganglion blocking effect), eliminates smooth muscle spasm , and reduces the excitability of the myocardium and motor zones of the cerebral cortex . When administered intravenously, it has analgesic, anti-shock, antihypertensive and antiarrhythmic effects (increases the effective refractory period, reduces excitability, automatism and conductivity), in large doses it can disrupt neuromuscular conduction. Eliminates the downward inhibitory effects of the reticular formation of the brain stem. Inhibits polysynaptic reflexes . In large doses, it can cause seizures . It has a short anesthetic activity (the duration of infiltration anesthesia is 0.5-1 hours). When administered intramuscularly, it is effective in elderly patients in the early stages of diseases associated with functional disorders of the central nervous system ( arterial hypertension , spasms of coronary and cerebral vessels, etc.)
Pharmacokinetics
It undergoes complete systemic absorption . The degree of absorption depends on the place and route of administration (especially on vascularization and blood flow velocity in the area of administration) and the total dose (amount and concentration). It is rapidly hydrolyzed by plasma and liver esterases with the formation of 2 main pharmacologically active metabolites : diethylaminoethanol (has a moderate vasodilating effect) and PABA (it is a competitive antagonist of sulfonamide chemotherapeutic drugs and can weaken their antimicrobial effect). T 1/2 - 30-50 s, in the neonatal period - 54-114 s. It is excreted mainly by the kidneys in the form of metabolites; not more than 2% is excreted unchanged.
Indications
Infiltration (including intraosseous), conduction, epidural, spinal anesthesia ; terminal (superficial) anesthesia (in otorhinolaryngology); vagosympathetic cervical and perinephral block, retrobulbar (regional) anesthesia. Rectal: hemorrhoids , anal fissures. Previously prescribed for such indications as gastric and duodenal ulcer, nausea, ulcerative colitis , itchy skin (atopic dermatitis , eczema ), keratitis , iridocyclitis , glaucoma .
Contraindications
Hypersensitivity (including to PABA and other local ether anesthetics). For anesthesia by the method of creeping infiltrate: pronounced fibrotic changes in the tissues; for subarachnoid anesthesia - AV block, bleeding, arterial hypotension , shock , infection of the site of lumbar puncture, septicemia . Caution: Emergency operations accompanied by acute blood loss, conditions accompanied by a decrease in hepatic blood flow (for example, heart failure, liver disease), progression of cardiovascular failure (usually due to the development of heart block and shock), inflammatory diseases or infection of the injection site, pseudocholinesterase deficiency, renal failure , childhood (up to 18 years), in elderly patients (over 65), seriously ill, debilitated patients, pregnancy , childbirth. For subarachnoid anesthesia: back pain, brain infections, benign and malignant neoplasms of the brain, coagulopathy , migraine , subarachnoid hemorrhage, arterial hypotension, skin paresthesias , psychosis , hysteria , non-contact patients, impossibility of puncture due to spinal deformity.
Dosage
For infiltration anesthesia 350-600 mg 0.25-0.5% solutions; for anesthesia according to the Vishnevsky method (tight creeping infiltration) - 0.125-0.25% solutions; for conduction anesthesia - 1-2% solutions (up to 25 ml); for epidural - 2% solution (20-25 ml); for the spinal - 5% solution (2-3 ml); for terminal anesthesia (in otorhinolaryngology) - 10-20% solution. To reduce absorption and lengthen action with local anesthesia, an additional 0.1% solution of epinephrine hydrochloride is added - 1 drop per 2-5-10 ml of procaine solution. In case of perinephral blockade (according to A. V. Vishnevsky ), 50–80 ml of a 0.5% solution or 100–150 ml of a 0.25% solution is injected into the perinephric tissue , and in case of vagosympathetic blockade, 30–100 ml of a 0.25% solution. A 10% solution is also used for electrophoretic administration. Higher doses for adult infiltration anesthesia: the first single dose at the beginning of the operation is not higher than 1 g of 0.25% solution (500 ml) and 0.75 g of 0.5% solution (150 ml). The maximum dose for use in children is up to 15 mg / kg. Rectally: having previously released the suppository from the contour packaging using scissors (cutting the packaging along the contour of the suppository), enter it deep into the anus (after a cleansing enema or spontaneous release of the intestine) 1-2 times a day. A novocaine solution is also used to dissolve the preparations according to the instructions of the drug with which it must be diluted.
Side Effects
From the central and peripheral nervous system
Headache, dizziness, drowsiness, weakness, motor anxiety, loss of consciousness, cramps, trismus , tremors , visual and auditory disorders, nystagmus , horse tail syndrome (leg paralysis , paresthesia), respiratory muscle paralysis, motor and sensory block, respiratory paralysis more often develops with subarachnoid anesthesia.
From the cardiovascular system
Increase or decrease in blood pressure , peripheral vasodilation , collapse , bradycardia , arrhythmias , chest pain.
From the urinary system
Involuntary urination.
From the digestive system
Nausea , vomiting , involuntary bowel movements .
Blood side
Methemoglobinemia .
Allergic reactions
Itching of the skin, skin rash, other anaphylactic reactions (including anaphylactic shock ), urticaria (on the skin and mucous membranes).
Others
Return of pain, persistent anesthesia, hypothermia , impotence ; with anesthesia in dentistry: numbness and paresthesia of the lips and tongue, lengthening of anesthesia.
Overdose
Symptoms
Pallor of the skin and mucous membranes, dizziness, nausea, vomiting, “cold” sweat, increased breathing, tachycardia , decreased blood pressure, up to collapse, apnea , methemoglobinemia. The action on the central nervous system is manifested by a sense of fear, hallucinations , convulsions, motor excitement.
Treatment
Maintaining adequate pulmonary ventilation with oxygen inhalation, intravenous administration of short-acting drugs for general anesthesia, in severe cases - detoxification and symptomatic therapy.
Special instructions
Patients require control of the functions of the cardiovascular system, respiratory system and central nervous system. It is necessary to cancel MAO inhibitors 10 days before the introduction of a local anesthetic. During the treatment period, care must be taken when driving vehicles and engaging in other potentially dangerous activities that require an increased concentration of attention and speed of psychomotor reactions.
Interaction
Local anesthetics increase the inhibitory effect on the central nervous system. Other anticoagulants ( ardeparin , dalteparin , danaparoid , enoxaparin , heparin , warfarin ) increase the risk of bleeding. When treating the injection site of local anesthetic with disinfectant solutions containing heavy metals, the risk of developing a local reaction in the form of pain and swelling increases . When using local anesthetics for spinal and epidural anesthesia with guanadrell , guanethidine , mecamylamine , trimethafan , the risk of a sharp decrease in blood pressure and bradycardia increases . Use with MAO inhibitors ( furazolidone , procarbazine , selegiline ) increases the risk of hypotension . Strengthen and lengthen the effect of muscle relaxant drugs. When prescribing procaine, along with narcotic analgesics, an additive effect is noted, which is used during spinal and epidural anesthesia, while respiratory depression is enhanced. Vasoconstrictors ( epinephrine , methoxamine , phenylephrine ) lengthen the local anesthetic effect. Procaine reduces the anti-myasthenic effect of drugs, especially when used in high doses, which requires additional correction of the treatment of myasthenia gravis . Cholinesterase inhibitors (anti-myasthenic drugs, cyclophosphamide , demecarin , ecothiophate , thiotepa ) reduce the metabolism of local anesthetics. The procaine metabolite (PABA) is an antagonist of sulfonamides.
Dosage Form
Ointment for external use, injection , rectal suppositories
In addition to the pure substance, there are combined preparations containing procaine, for example, sulfocamphocaine.
Links
- Chemical Encyclopedic Dictionary I.L. Knunyants. - M .: Owls. Encyclopedia, 1983-792 p.