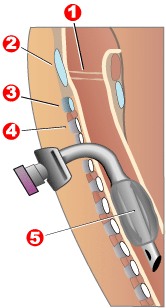
1 - Vocal cords
2 - Thyroid cartilage
3 - Cricoid cartilage
4 - Tracheal cartilage
5 - balloon cuff
Tracheostomy ( Latin tracheostomia , from other Greek. Τραχεῖα - respiratory throat and στóμα - hole, passage) - a surgical operation to form a temporary or persistent anastomosis of the tracheal cavity with the environment ( stoma - fistula ), carried out by introducing a cannula into the trachea or hemming tracheal wall to the skin . The result is the flow of air into the respiratory tract.
Tracheostomy is performed most often for health reasons, in a planned or urgent manner.
Content
- 1 Indications
- 2 Classification
- 3 Instrumentation for tracheostomy
- 4 Technique
- 5 Errors and complications
- 6 Famous people who have undergone a tracheostomy
- 7 Notes
- 8 References
Indications
1. Successful or threatening obstruction of the upper respiratory tract
- The sharpest (lightning fast) . Develops in seconds. As a rule, this is obstruction by foreign bodies
- Sharp . Develops in minutes. Foreign bodies, true croup for diphtheria (obturation with films), Quincke's edema , less often - ligamentous laryngitis
- Subacute . Develops in tens of minutes, hours. False croup , laryngeal tonsillitis, edema with chemical burns of the esophagus, etc.
- Chronic It develops in a day, months, years. Perichondritis, cicatricial narrowing of the trachea, cancer of the larynx
Most often, the following conditions lead to obstruction of the upper respiratory tract:
- Foreign bodies of the respiratory tract (if it is impossible to remove them with direct laryngoscopy and tracheobronchoscopy);
- Violation of the airway during injuries and closed injuries of the larynx and trachea ;
- Acute stenosis of the larynx in infectious diseases ( diphtheria , influenza, whooping cough , measles , rash or recurrent typhoid, erysipelas);
- Laryngeal stenosis with specific infectious granulomas (tuberculosis, syphilis, scleroma, etc.);
- Acute stenosis of the larynx in non-specific inflammatory diseases (abscessed laryngitis, laryngeal tonsillitis, false croup);
- Laryngeal stenosis caused by malignant and benign tumors (rarely);
- Compression of the tracheal rings from the outside by the jet, aneurysm, inflammatory neck infiltrates;
- Stenoses after chemical burns of the mucous membrane of the trachea with acetic essence, caustic soda, fumes of sulfuric or nitric acid, etc .;
- Allergic stenosis (acute allergic edema);
2. The need for respiratory support in patients undergoing prolonged mechanical ventilation
It is necessary for severe traumatic brain injury, for poisoning with barbiturates, for a burn disease, ALS (amyotrophic lateral sclerosis), etc.
Classification
- According to the level of dissection of the trachea relative to the isthmus of the thyroid gland, upper, middle and lower tracheostomy are distinguished.
- In the direction of the tracheal incision - longitudinal, transverse, U-shaped (according to Björk) tracheostomy.
Adults have an upper tracheotomy, children have a lower one, since their thyroid gland is located higher. Secondary tracheotomy is extremely rare if it is not possible to produce an upper or lower tracheotomy, for example, with a special anatomical variant of the location of the thyroid gland or with a thyroid tumor.
Tracheostomy Instrumentation
- A set of general surgical instruments: hats, anatomical tweezers, surgical tweezers, Billroth and Kocher styptic clamps , a scalpel , straight and Cooper scissors, sharp hooks, blunt hooks, a grooved probe, an elastic catheter for suctioning blood, a syringe suitable for a catheter, or surgical a pillow with oxygen, needle holders, 10-15 needles of various numbers.
- Special tools for tracheostomy:
- Tracheostomy cannulas. The most widely used Luer cannula, which consists of two tubes - external and internal. The modern design consists of metal rings and is arranged as a corrugated tube;
- Shassignyak sharp single-tooth tracheostomy hook, designed to fix the trachea;
- Dull hook to move the isthmus of the thyroid gland;
- A tracheodilator to expand the edges of the tracheal incision before the cannula is inserted into its lumen. The most widespread are the tracheo expanders Trousseau (1830) and S.I. Wulfson (1964).
- Shassignyak sharp single-tooth tracheostomy hook, designed to fix the trachea;
Execution Technique
The patient lies on his back, a roller is placed under his shoulders, his head is thrown back. This position of the patient allows you to maximize bring the larynx and trachea to the front of the neck. The operation is performed both under endotracheal anesthesia and under local anesthesia. In children, endotracheal anesthesia is usually used. Local infiltration anesthesia is performed with 0.5-1% novocaine solution or 0.5% trimecaine solution. Under extreme conditions, they operate without anesthesia.
- Technique of the upper tracheostomy.
A layer-by-layer incision is made of the skin, subcutaneous tissue, superficial fascia and white line of the neck 4-6 cm long from the thyroid cartilage down, after which the sterno-thyroid muscle (m.sternothyroideus) of the right and left halves of the neck is exposed. Spreading the muscles, they find the cricoid cartilage and the isthmus of the thyroid gland lying under it. Dissect the leaf of the intracervical fascia (f.endocervicalis) in the transverse direction, after which the isthmus is separated from the trachea and pushed it bluntly downward, thus exposing the upper cartilage of the trachea. After that, the larynx is fixed with a single-pointed pointed hook to stop convulsive movements. Taking the pointed scalpel in the hand with the blade up, the operator places the index finger on the side of the blade and, not reaching the tip of 1 cm (in order not to damage the back wall of the trachea, opens the third, and sometimes the fourth, cartilage of the trachea, directing the scalpel from the isthmus to the larynx (up). After air enters the trachea, breathing stops for a while, apnea occurs, followed by a sharp cough, and only after that the tracheodilator is inserted into the tracheotomy wound, and the tracheostomy cannula is removed and placed across the trachea so that the flap is in the sagittal plane, draw into the lumen of the trachea, the expander is removed, the cannula is rotated so that the flap is located in the frontal plane, followed by the cannula moving down and fixing it around the neck.The skin wound is sutured to the tracheostomy tube.
- Technique of the lower tracheostomy.
The incision is carried out from the cricoid cartilage to the sternum. Dissect the surface leaf of the own fascia of the neck and penetrate into the suprasternal interaponeurotic space (spatium interaponeuroticum suprasternale). In a blunt way, the cellulose is separated and, moving down the venous jugular arch, a deep leaf of the own fascia of the neck (scapular-clavicular fascia) is cut and the muscles (sternum-hyoid and sternum-thyroid) of the right and left halves of the neck are exposed. Spreading the muscles to the sides, dissect the parietal plate of the intracervical fascia (f. Endocervicalis) and penetrate into the pre-tracheal space. In the fiber of this space, the venous plexus and sometimes the lower thyroid artery (a. Thyroidea ima) are found. The vessels are ligated and transected, and the isthmus of the thyroid gland is pulled up. The trachea is freed from the visceral fascia fascia covering it and the fourth and fifth tracheal cartilages are dissected. The scalpel must be held as described above and directed from the sternum to the isthmus so as not to damage the brachiocephalic trunk. Further methods are no different from those indicated for the upper tracheostomy.
- Technique of cryoconicotomy.
- At the same time, a vertical incision along the midline of the neck below the thyroid cartilage dissects the skin, the arch of the cricoid cartilage and the thyroid cricoid ligament;
- Introduce a clamp into the incision and push the branches apart, which ensures the flow of air into the respiratory tract;
- After the disappearance of asphyxia, a cryoconicotomy is replaced by a tracheostomy.
Errors and Complications
Like any major surgery, a tracheostomy has its own complications. Their severity ranges from cosmetic defects to death. Moreover, the more time has passed after the operation, the less the likelihood of serious complications.
- Complications that may occur during the operation: in
- An incision made not along the midline of the neck can lead to damage to the cervical veins, and sometimes to the carotid artery (one should not forget about the possibility of air embolism in case of damage to the cervical veins).
- Insufficient hemostasis before opening the trachea can lead to leakage of blood in the bronchi and the development of asphyxiation.
- If possible, the tracheal incision should correspond to the diameter of the cannula .
- Injury to the posterior wall of the esophagus.
- Before the introduction of the cannula, you should make sure that the mucous membrane of the trachea is dissected and its lumen is opened, otherwise you can insert the cannula into the submucosal layer, which will lead to a protrusion of the mucous membrane into the lumen of the trachea and increased asphyxiation .
- Insufficient hemostasis before opening the trachea can lead to leakage of blood in the bronchi and the development of asphyxiation.
- Complications, the occurrence of which is possible immediately after the operation: there is a risk of hypoxia, perforation of the posterior wall of the trachea, fracture of the tracheal ring, wound of the esophagus, subcutaneous emphysema , pneumothorax .
- In the later postoperative period, purulent tracheobronchitis, tracheal stenosis , tracheal fistula, voice changes, and, due to cosmetic complications, gross scars on the skin in the area of the tracheostomy can occur.
A large number of complications after a tracheostomy occurs as a result of blockage of the tube, mismatch of its size and trachea, incorrect position of the tube in the trachea, its displacement and loss.
Famous Tracheostomy
- Ayrton Senna
- John Paul II
- Frederick III
- Stephen Hawking
- Mika Hakkinen
- Elizabeth Taylor
- Peter Strum ( Saw 5 )