Kidney transplantation is a surgical operation that involves transplanting a kidney to a person or animal from another person or animal ( donor ). It is used as a method of renal replacement therapy in the terminal stage of chronic renal failure in humans and some animals (dogs and cats).
The most common variant of modern kidney transplantation in humans is heterotopic, allogeneic (from another person). As of September 1, 2009, 80,888 people are on the kidney transplant waiting list in the United States. In 2008, the United States performed 16517 kidney transplants and 837 liver and pancreas transplants.
History
For the first time in history, a kidney transplant in an animal was performed by the Hungarian surgeon Emmerich Ulmann in 1902. Regardless of him, experiments on kidney transplantation, its preservation, and the technique of applying vascular anastomoses were performed by Alexis Carrel in 1902–1914. He developed the basic principles of preservation of the donor organ, its perfusion. Alexis Carrel was awarded the Nobel Prize in 1912 for work on organ transplantation. Apparently, the first attempt at organ transplantation from an animal to a man was made by Mathieu Jabouille, who transplanted a pig kidney to a patient with nephrotic syndrome, which ended fatally. In the early years of the 20th century, other attempts were made to transplant organs from animals (pigs, monkeys) to people, also unsuccessful. In 1931, in Kharkov [1] [2], Yu. Yu. Voronoi for the first time in the world made an attempt to transplant a kidney from person to person [3] . He transplanted a kidney from the corpse of a 60-year-old man who had died 6 hours earlier, to a young woman, 26 years old, who had taken mercury chloride for suicidal purposes. The kidney was transplanted as a temporary measure for the period of the anuric phase of acute renal failure, in the patient's hip area. Unfortunately, Voronoi had no data on kidney viability after a long thermal ischemia , which led to a naturally unsuccessful result of the operation, the patient died.
Only the appearance in 1943 of the works of Peter Medawar in the field of tissue immunology and tissue compatibility allowed the first attempts to be made on truly scientifically based transplantations. In 1950, R. Lawler in Chicago performs orthotopic kidney transplantation. Instead of a removed polycystic kidney, he transplanted a 44-year-old woman to the same place a kidney from a corpse of the same blood type. The transplant lasted 53 days. In 1951, Charles Dubost in Paris tried to transplant a headless criminal's kidney into a patient with acute renal failure in the iliac fossa. Confidently, the staff of the Peter Bent Brayham Clinic in Boston went on to perform kidney transplantation. In 1947, David Hume, Charles Hafnagel and Ernest Landsteiner (the son of Karl Landsteiner, a blood-type explorer) performed a temporary kidney transplant for a young girl with acute renal failure due to an infected abortion . The kidney is sewn to the vessels of the forearm. Despite the fact that the transplant began to function, against which the function of its kidneys was restored, the patient died from acute hepatitis , which complicated blood transfusion. The first successful kidney transplant was a related kidney transplant performed by Joseph Murray and the same surgeons under the guidance of therapist John Merill. On October 26, 1954, a young man, Richard Herrick, was hospitalized with kidney failure. He had a twin brother, Ronald. After stabilizing Richard's condition, a team of surgeons performed a test skin transplant between brothers in order to confirm the identity of their tissue phenotypes . There was no rejection. On December 23 of the same year, a kidney transplant was performed with immediate graft function. Richard lived 9 years after surgery and died from a relapse of the underlying disease. Ronald died on December 29, 2010. Subsequent kidney transplants between twin brothers were also successful. In 1959, the first kidney transplant was performed from a posthumous unrelated donor. To suppress immunity, total body irradiation was used. The recipient lived after surgery for 27 years.
In 1960, Schwartz and Dameschek described in an experiment the immunosuppressive effect of 6-mercaptopurine. On its basis, the drug azathioprine is being developed, which allows transplantation from unrelated donors. On December 31, 1972, Hartmann Stekhelin opens a new immunosuppressive drug cyclosporin , first successfully used in the clinic by Thomas Starzl in 1980. This ushered in a new era in transplantation. In 1990, another immunosuppressive drug, tacrolimus, was developed at the University of Pittsburgh under the leadership of Starzl.
Indications
An indication for kidney transplantation is terminal chronic renal failure (ESRD, ICD code N 18.0) - the final stage of the course of chronic glomerulonephritis, chronic pyelonephritis, diabetic nephropathy, polycystic kidney disease, injuries and urological diseases, congenital kidney diseases. Patients with ESRD are undergoing renal replacement therapy (RRT) to save life, which includes chronic hemodialysis , peritoneal dialysis, and kidney transplantation. Compared to the other two options, kidney transplantation has the best results in terms of life expectancy (increasing it by 1.5-2 times compared with other options for renal replacement therapy), its quality. Kidney transplantation is a method of choice in children, since the development of the child on hemodialysis is significantly affected.
Contraindications
In modern conditions, there is no single view of contraindications for kidney transplantation and the list of contraindications for transplantation may differ in different centers. The most common contraindications for kidney transplantation include the following.
- The presence of a cross-immunological reaction with donor lymphocytes (cross match) . An absolute contraindication to transplantation, the presence of a reaction is associated with an extremely high risk of super-acute transplant rejection and loss.
- Malignant neoplasms , currently available or with a short period after radical treatment. In the case of a radical cure, with most tumors, at least 2 years should elapse from the completion of such treatment. They do not wait any time after successful treatment of asymptomatic kidney tumors, in situ bladder cancer, in situ cervical cancer, basal cell carcinoma. The observation period is increased to 5 years after treatment of invasive cancer of the cervix, melanoma, and breast cancer.
- Active infections . With cured tuberculosis, it is necessary to monitor the patient for at least a year. HIV infection is an absolute contraindication to a kidney transplant in most transplant centers. The presence of chronic inactive hepatitis B, C is not a contraindication to surgery.
- Emergency diseases in the stage of decompensation , which may threaten in the postoperative period, for example, an active stomach ulcer or decompensated heart failure.
- Non-compliance by the patient with medical recommendations and lack of discipline ( incompliance ). In the world, about 5-10% of transplant losses are due to the fact that patients do not fulfill the prescriptions prescribed by the doctor regarding immunosuppressive therapy regimen.
- Personality changes in chronic psychoses, drug addiction and alcoholism, which do not allow the patient to comply with the prescribed regimen.
At present, diabetes mellitus (leading to diabetic nephropathy and terminal kidney damage) is no longer considered a contraindication to transplantation. Diabetic patients have a slightly lower percentage of transplant survival, but with modern treatment, this result is increasingly improved.
Donor Stage
A kidney transplant can be obtained from living related donors or cadaver donors. The main criteria for selecting a transplant is the correspondence of blood groups AB0 (some centers perform transplantation without taking into account group affiliation), HLA alleles (usually A, B, Dr), approximate correspondence of the weight, age and gender of the donor and recipient. Donors should not be infected with vector-borne infections (syphilis, HIV, hepatitis B, C). Currently, against the background of a worldwide shortage of donor organs, donor requirements are being reviewed. So, more often, donated elderly patients with diabetes mellitus, who had a history of arterial hypertension, episodes of hypotension in the agonal and pre-agonal period began to be considered as donors. Such donors are called marginal or extended criteria donors. The best results are achieved with kidney transplantation from living donors, but most patients with chronic renal failure, especially adults, do not have sufficiently young and healthy relatives who can donate their organ without harm to health. Post-mortem organ donation is the only way to provide transplantation care for the majority of patients who need it. Live kidney donors undergo laparoscopic donor nephrectomy and open donor nephrectomy. Post-mortem donors (on a corpse) undergo kidney transplant explantation operations in isolation or as part of a multi-organ transplant organ harvesting operation.
After or during the removal of the renal transplant, its cold pharmacoconservation is performed. To maintain the viability of the donor organ, it must be washed from the blood and perfused with a preservative solution. The most common at present are solutions of Brettschneider (Custodiol), Collins (EuroCollins), University of Wisconsin (UW, Viaspan). Most often, the transplant is stored according to the non-perfusion method in the “triple bags” system - the organ washed with the preserving solution is placed in a sterile plastic bag with preservative, this bag is placed in another bag filled with sterile snow porridge (sludge), the second bag is in the third one with ice-cold physiological saline. The organ in triple bags is stored and transported in a thermal container or refrigerator at a temperature of 4-6 ° C. Most centers determine the maximum period of cold ischemia (from the beginning of the preservation of the graft to the start of blood flow in it) at 72 hours, but the best results are achieved with kidney transplantation in the first day after its removal. The perfusion technique for storing a donor kidney, developed in 1906 by Alexis Carrell and Charles Lindberg, is sometimes used. In this case, the organ is connected to a machine that carries out a constant pulsation washing of the organ with a preservative solution. Such storage increases costs, but can improve the outcome of transplantation, especially when using kidneys from marginal donors.
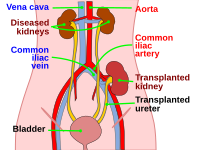
Recipient phase
In modern conditions, heterotopic transplantation is always performed. The graft is placed in the iliac fossa. Regarding the choice of the side for transplantation, there are several approaches. Due to the more superficial location of the iliac vein, the right side is more preferable for transplantation, therefore, in some centers the right side is always used, except for patients with an ultralaterally located peritoneal catheter, with a subsequent pancreas transplantation planned, with repeated transplantation. However, most often the right kidney is transplanted to the left, left to right, which is more convenient in the formation of vascular anastomoses . As a rule, the kidney is located in the retroperitoneal tissue, but in some cases the intraperitoneal location of the graft is used - in young children, after numerous previously performed transplants. The usual location of the kidney is in the iliac fossa. In this case, the arterial anastomosis is superimposed with the iliac arteries (internal, external or common), venous with the iliac veins, and the urinary bladder. However, in the presence of cicatricial changes, urological pathology, sometimes the organ is placed in the retroperitoneal space above. In this case, the arterial anastomosis is superimposed with the aorta, venous with the inferior vena cava. Urinary anastomosis is imposed by connecting the patient's ureter with the pelvis of the graft. Usually the patient’s own kidneys are not removed, except in the following cases:
- the size or position of their own kidneys interferes with the placement of the graft
- patients with polycystic kidney disease have large cysts that cause suppuration or bleeding
- high nephrogenic hypertension resistant to conservative treatment
Access . Pararectal arched or club-shaped incision. It starts almost from the midline 2 fingers above the pubis and goes up and out, following slightly outside the rectus abdominis muscles. Muscles are crossed by an electric knife. The lower epigastric artery in the lower abdominal wall intersects between two ligatures. The round ligament of the uterus intersects, and the spermatic cord is taken to the holder and retracted medially. The peritoneal sac moves medially. Naked by m.psoas. The vascular bundle is mobilized. When isolating blood vessels, it is necessary to carefully bandage and cross the lymph vessels that entangle the iliac bundle. Otherwise, lymphorrhea develops in the postoperative period. The ileal bundle is allocated and revised. Most often, an internal iliac artery is used for transplantation. It is allocated to a fork (trifurcation), the branches are bandaged and stitched. The artery under the DeBakey-Block block is crossed. The external iliac vein is mobilized. For convenience, it is good to install annular retractors into the wound.
Back table . The donor organ is removed from the bags into a tray with sterile snow. The artery and vein of the transplant are isolated and treated, the lateral branches are ligated. Excess tissue is removed, retaining fat in the pelvis, gently process the ureter, preserving its fiber.
Stage of imposition of vascular anastomoses . It is preferable to apply the venous anastomosis first, as it is located deep in the wound. For its formation, various technical methods are used, for example, the application of an anastomosis in 2 threads or in 4 threads. After the anastomosis is applied, the vein in the gate is pinched, the blood flow is launched. Next, an arterial anastomosis is formed at the site of Carrel. Anastomosis is formed by the parachute method or the usual continuous suture in 2 threads. A microsurgical technique is used to turn on additional arteries. They can be sutured both into the main trunk and vascularized using epigastric arteries. After the completion of vascular anastomoses, blood flow is turned on. With a small cold ischemia after the start of blood flow from the ureter, urine begins to flow.
The stage of application of the urinary anastomosis . Most often, an anastomosis of the ureter transplant with the recipient's bladder according to Litch or Ledbetter-Politano is applied. The bubble is inflated with air or a sterile solution. In the bottom, muscles are dissected, a continuous anastomosis with the mucous membrane of polydioxanone is superimposed. After that, the muscle layer of the bladder is sutured in order to form an antireflux valve. Good results are achieved when S or J-shaped ureteral stents (urecath) are placed in place of the anastomosis.
Graft placement . The graft is placed so that the vein of the kidney is not twisted, the artery makes an arch, and the ureter lies freely and does not bend.
Exit the operation . The graft bed is drained by one thick tube, to which the active drainage is connected according to Redon. Layered seams on the wound. Since in the postoperative period the patient will receive steroids in large doses, it is preferable to apply a cosmetic suture on the skin.
Surgical Complications
- Bleeding
- Transplant Artery Thrombosis
- Transplant rupture
- Graft artery stenosis
- Recipient ileal artery thrombosis
- Venous thrombosis
- Venous thromboembolism
- Aneurysms and fistulas
- Urological complications - failure of the urinary anastomosis, obstruction of the urinary tract, hematuria
- Lymphocele
- Wound failure
- Wound infection
Notes
- ↑ The Charity Fund of the Name of George Voronoi - The Younger Son of Voronoi G.F. . voronuy.at.ua. Circulation date May 2, 2019.
- ↑ “The kidneys of fresh corpses are able to come to life” . Newspaper.Ru. Circulation date May 2, 2019.
- ↑ Klyap S.I. Yu. Yu. Voronoi and his role in the development of kidney transplantation . Blagodarny Fund imeni George Voronoi. Date of treatment January 31, 2014.
Literature
- Колсанов А. В., Харитонов Б. И., Иванова В. Д., Миронов А. А., Яремин Б. И., Юнусов Р. Р., Бардовский И. А. Вопросы трансплантации органов . — Самара: ГОУ ВПО СамГМУ Минздравсоцразвития России. — 2008.
- Трансплантация почки. Национальные клинические рекомендации. Москва, 2013.
- Буржи А., Аун Р. и др. Опыт трансплантации почек: типичные и атипичные показания. Per. from English Н. Д. Фирсовой (2018).