Toxoplasmosis is a parasitic disease in humans and animals caused by Toxoplasma gondii toxoplasma , which in the vast majority of cases is asymptomatic [3] . The source of invasion is various species (over 180) of domestic and wild mammals ( cats , dogs , rabbits ; predators , herbivores , rodents ).
| Toxoplasmosis | |
|---|---|
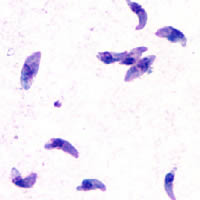 Toxoplasma with optical microscopy | |
| ICD-10 | B 58. |
| ICD-10-KM | and |
| ICD-9 | 130 |
| ICD-9-KM | , and |
| Diseasesdb | 13208 |
| Medlineplus | 000637 |
| eMedicine | med / 2294 |
| Mesh | and |
Content
Epidemiology
Up to half of the world's population is infected with toxoplasmosis [4] . In the USA, carriers are 23% of the population [5] , in Russia - about 20% [6] , and in some parts of the world the proportion of carriers reaches 95% [7] .
The global annual incidence of congenital toxoplasmosis is estimated at 190,100 cases. High levels of the disease have been reported in South America , some Middle Eastern and low-income countries [8] .
Ways of infection
Human infection occurs when meat products and eggs that have not undergone sufficient heat treatment are consumed. The possibility of infection if the pathogen enters the mucous membranes and damaged skin, is possible by a vector-borne transmission (see Vector-borne diseases ). There is also intrauterine infection. Factors that can contribute to the appearance of a parasite in the body and increase the risk of toxoplasmosis:
- contact with infected animals;
- the use of unwashed cat litter after cleaning the cat’s toilet or any other contact with cat feces;
- eating raw or not fully cooked meat, especially pork, beef, lamb or venison;
- contact with raw or unroasted meat;
- organ transplantation or blood transfusion (very rare);
- the presence of toxoplasmosis in parents.
Clinical picture
There are congenital and acquired (acute and chronic) toxoplasmosis. With congenital toxoplasmosis, fetal death in the womb, death of a newborn as a result of a general infection or (in survivors) damage to the nervous system, eyes and other organs, oligophrenia are observed . Oligophrenia in congenital toxoplasmosis reaches a severe degree and manifests itself from the first months of life [9] .
The acute acquired form occurs as a typhoid- like disease (with high fever, enlarged liver, spleen) or with a predominant lesion of the nervous system (headache, convulsions, vomiting , paralysis, etc. [ what? ] ). More often, toxoplasmosis proceeds chronically, with subfebrile temperature , headache, enlarged lymph nodes and liver, decreased performance; may be accompanied by damage to the eyes, heart, nervous and other systems and organs. Toxoplasmosis can occur in latent (latent) form.
Diagnostics
The main method for diagnosing the disease is serological .
Determination of the level of immunoglobulins G by ELISA or indirect fluorescence.
The level of antibodies reaches its maximum level 1-2 months after the onset of the disease and subsequently is recorded indefinitely .
In patients with seroconversion or a four-fold increase in IgG titer, the level of specific IgM is determined to confirm the presence of acute infection.
ELISA is the method of choice in the analysis of IgM levels; with its help, an increase in their concentration is recorded 2 weeks after infection.
The peak concentration of antibodies is reached after a month, they usually disappear after 6–9 months, but in some cases they can be periodically detected for 2 years or more, making it difficult to differentiate between acute and chronic forms of infection .
Treatment
Ordinary people are cured of the acute form of toxoplasmosis on their own, without medical treatment. Pregnant women and newborns need treatment, but it should be understood that the goal of treatment is only to eliminate the acute phase and symptoms of the disease. Persons with an ocular form of the disease should be treated by an ophthalmologist and receive drugs prescribed depending on the size of the lesion and its form: acute or chronic (without progression). Persons with weakened immunity (for example, with HIV ) should receive treatment until the signs of the disease are eliminated, and patients in the AIDS stage receive treatment for toxoplasmosis for life [10] .
Treatment is usually required only for people with serious health problems, for example, people with HIV who have a CD4 count of less than 200 cells in mm³ of blood, because the disease is usually only dangerous when the immune system is weak. Co-trimoxazole (Biseptol) is the drug of choice to prevent toxoplasmosis, but it is not suitable for the treatment of the active form of the disease. A new study (May 2012) shows a promising way to treat the active and latent forms of this disease using two [ what? ] antimalarial drugs of the ELQ class (Endochin-like quinolones) [11] .
Sharp form
The following drugs are indicated for the treatment of acute toxoplasmosis [12] :
- Pyrimethamine (Daraprim) - an anti- malarial medicine;
- Sulfadiazine (Argedin) - an antibacterial drug from the group of sulfonamides used in combination with pyrimethamine to treat toxoplasmosis;
- Combination therapy is usually performed with folic acid to reduce the risk of thrombocytopenia .
- Combination therapy is most useful in the presence of HIV.
- Clindamycin ( Dalacin and others) is a semi-synthetic antibiotic of the linkosamide group;
- Spiramycin ( Doramycin and others) is a natural macrolide antibiotic used most often for pregnant women in order to prevent infection of the fetus.
Other antibiotics, such as minocycline (Minolexin and others), are used as reserve drugs, that is, if the usual methods of treatment do not help or are contraindicated for some reason.
Latent form
In people with latent toxoplasmosis, toxoplasma cysts are resistant to treatment, since antibiotics do not reach bradisiot in sufficient concentration. Medications prescribed for the latent form of toxoplasmosis:
- Atovaquone (Mepron) is an antibiotic that is used to kill toxoplasma cysts in HIV patients;
- Clindamycin (Dalacin and others) is a semi-synthetic antibiotic of the lincosamide group, which in combination with Atovaquone seems to be optimal for the destruction of toxoplasma cysts in mice.
Congenital Toxoplasmosis
In the event that a pregnant woman is ill with acute toxoplasmosis, amniocentesis can be used to determine if the fetus has been infected. When a pregnant woman becomes ill with acute toxoplasmosis, there is an approximately 30 percent chance that toxoplasma tachyzoites will infect the placental tissue, and the fetus will also become infected from there [13] .
If the parasite has not yet reached the fetus, Spiramycin may help prevent transmission through the placenta. If the fetus has been infected, a pregnant woman can be treated with pyrimethamine and sulfadiazine after the first trimester, with the addition of folic acid. This is done after the first trimester, since pyrimethamine has an anti-folate effect, and the absence of folic acid in the first trimester can interfere with the formation of the fetal brain and cause thrombocytopenia [14] . Infection at earlier stages of pregnancy correlates with worsening fetal and neonatal prognoses [15] .
Forecast
In individuals without immunodeficiency, it is usually favorable.
When infected with toxoplasma in the presence of pregnancy, or less than 3-9 months before it, the prognosis is negative for the fetus. When infected in the first trimester of pregnancy, there is a high risk of deviations incompatible with life. When infected in the second trimester, there is a high probability of pathologies of the brain, nervous system, and organs of vision. When infected in the third trimester of pregnancy, the chance of infection of the baby is high, but the consequences are less dangerous and may be absent or appear in latent form [6] [16] [17] [18] .
Prevention
The fight against toxoplasmosis of domestic animals, compliance with sanitary rules when caring for animals and processing products, a thorough examination of pregnant toxoplasmosis. Toxoplasma in meat dies when the meat is heated to 67 ° C or cooled to −13 ° C [19] .
Notes
- ↑ 1 2 Disease Ontology release 2019-05-13 - 2019-05-13 - 2019.
- ↑ 1 2 3 Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018.
- ↑ Hunter CA , Sibley LD Modulation of innate immunity by Toxoplasma gondii virulence effectors. (Eng.) // Nature reviews. Microbiology. - 2012. - Vol. 10, no. 11 . - P. 766-778. - DOI : 10.1038 / nrmicro2858 . - PMID 23070557 .
- ↑ Flegr J. , Prandota J. , Sovičková M. , Israili ZH Toxoplasmosis - a global threat. Correlation of latent toxoplasmosis with specific disease burden in a set of 88 countries. (English) // Public Library of Science ONE. - 2014 .-- Vol. 9, no. 3 . - P. e90203. - DOI : 10.1371 / journal.pone.0090203 . - PMID 24662942 .
- ↑ Jones JL , Parise ME , Fiore AE Neglected parasitic infections in the United States: toxoplasmosis. (English) // The American journal of tropical medicine and hygiene. - 2014 .-- Vol. 90, no. 5 . - P. 794-799. - DOI : 10.4269 / ajtmh.13-0722 . - PMID 24808246 .
- ↑ 1 2 G. Yu. Nikitina, L.P. Ivanova, S. Kh. Zembatova, F.K. Dzutseva, Yu. V. Borisenko. Features of the diagnosis and treatment of toxoplasmosis in pregnant women . Attending physician (November 2011).
- ↑ Parasites - Toxoplasmosis (Toxoplasma infection) . Epidemiology & Risk Factors . Centers for Disease Control and Prevention (March 26, 2015) . Date of treatment September 23, 2015. Archived April 24, 2015.
- ↑ Paul R Torgerson & Pierpaolo Mastroiacovo. The global burden of congenital toxoplasmosis: a systematic review . . Bulletin of the World Health Organization , Issue 91, No. 7, pp. 465-544 (July 7, 2013) . Date of treatment September 23, 2015.
- ↑ Isaev D.N. Mental retardation in children and adolescents. Leadership. - St. Petersburg: Speech, 2003 .-- S. 63. - 397 p. - ISBN 5-9268-0212-1 .
- ↑ Parasites - Toxoplasmosis (Toxoplasma infection) . Treatment Centers for Disease Control and Prevention (10 January 2013) . Date of treatment September 23, 2015. Archived July 27, 2015.
- ↑ Doggett JS , Nilsen A. , Forquer I. , Wegmann KW , Jones-Brando L. , Yolken RH , Bordón C. , Charman SA , Katneni K. , Schultz T. , Burrows JN , Hinrichs DJ , Meunier B. , Carruthers VB , Riscoe MK Endochin-like quinolones are highly efficacious against acute and latent experimental toxoplasmosis. (Eng.) // Proceedings of the National Academy of Sciences of the United States of America. - 2012. - Vol. 109, no. 39 . - P. 15936-15941. - DOI : 10.1073 / pnas . 1208069109 . - PMID 23019377 .
- ↑ Parasites - Toxoplasmosis (Toxoplasma infection) . Resources for Health Professionals . Centers for Disease Control and Prevention (April 14, 2014) . Date of treatment September 23, 2015. Archived September 23, 2015.
- ↑ Robert-Gangneux, F .; Darde, M.-L. Epidemiology of and Diagnostic Strategies for Toxoplasmosis (English) // Clinical Microbiology Reviews : journal. - 2012. - Vol. 25 , no. 2 . - P. 264-296 . - ISSN 0893-8512 . - DOI : 10.1128 / CMR.05013-11 .
- ↑ Jones J. , Lopez A. , Wilson M. Congenital toxoplasmosis. (Eng.) // American family physician. - 2003. - Vol. 67, no. 10 . - P. 2131-2138. - PMID 12776962 .
- ↑ McLeod R. , Kieffer F. , Sautter M. , Hosten T. , Pelloux H. Why prevent, diagnose and treat congenital toxoplasmosis? (Eng.) // Memorias do Instituto Oswaldo Cruz. - 2009. - Vol. 104, no. 2 . - P. 320—344. - PMID 19430661 .
- ↑ What are the risks of toxoplasmosis during pregnancy? / NHS Choises, 05/03/2014
- ↑ Parasites - Toxoplasmosis (Toxoplasma infection) - Pregnant Women // CDC, March 26, 2015 (eng.)
- ↑ Toxoplasmosis in Pregnancy: Prevention, Screening, and Treatment / J Obstet Gynaecol Can 2013; 35 (1 eSuppl A): S1-S7
- ↑ Topley, 2007 , p. 439.
Literature
- Kazantsev A.P. Toxoplasmosis . - L .: Medicine . Leningra. Department, 1985 .-- 168 p. - (Practitioner Library: Infectious and Parasitic Diseases). - 20,000 copies.
- Topley and Wilson's microbiology and microbial infections. Parasitology / Edited by Francis EG Cox, Derek Wakelin, Stephen H. Gillespie, Dickinson D. Despommier. - Hodder Arnold, 2007. - T. 6. - ISBN 9780340885680 .
Links
- Toxoplasmosis - Recent advances, Open access book published in September 2012
- Valery Viktorovich Vasiliev. Toxoplasmosis: modern scientific and practical approaches , 2001