Bronchopulmonary dysplasia (BPD) is a chronic disease that develops in premature infants due to mechanical ventilation of the lungs , which is based on damage to underdeveloped bronchi and lungs by high pressure, volume and oxygen, and manifested by tachypnea , dyspnea , hypoxemia , persistent obstructive disorders and radiological changes.
| Bronchopulmonary dysplasia | |
|---|---|
| ICD-10 | P 27.1 |
| ICD-10-KM | |
| ICD-9 | 770.7 |
| Diseasesdb | 1713 |
| Medlineplus | |
| eMedicine | ped / 289 |
| Mesh | D001997 |
Content
- 1 Definitions and diagnostics
- 2 Brief historical background
- 3 Epidemiology
- 4 Etiology
- 5 Clinic
- 5.1 Treatment
- 5.2 Rehabilitation
- 5.3 Prevention
- 6 Forecast
- 7 Notes
Definitions and Diagnostics
- Clinical definition
The criterion for the diagnosis of BPD is the need for oxygen at 36 weeks of adjusted gestational age. It is proved that the need for oxygen at 36 weeks post-conceptual age is a predictor of long-term impaired pulmonary function. The disadvantage of this definition is its subjectivity in the approach to determining oxygen demand, which allows significant variability in the frequency of diagnosis of BPD in various institutions.
- Physiological determination of BPD
Some authors (Michele C. Walsh et al.) Have shown that for unification and more accurate diagnosis of BPD, it is possible to use a sample with room air. It is proposed to diagnose BPD with a saturation of less than 90% after 30 minutes of breathing with room air. Thus, one can speak of true oxygen dependence, in contrast to the subjectively determined oxygen demand.
Brief historical background
The term BPD was proposed by WJ Northway in 1967 on the basis of observation and analysis of radiographs and pathological anatomical findings of 32 premature infants undergoing mechanical ventilation. BPD criteria were proposed by E. Bankalary in 1979. Initially, children after respiratory distress syndrome of the newborn (RDS of the newborn), after mechanical ventilation and inhalation of 80-100% oxygen for more than 150 hours (formula A. Philip (1975): oxygen + pressure + time). Definition of Bankalary - mechanical ventilation during the first 3 days of life, NAM at the age of 28 days. The appearance of the term “new BPD” is a consequence of the pathomorphism of the disease.
1) Oxygen-dependent BPD 2) Oxygen-independent BPD
Epidemiology
Etiology
The etiology of BPD is based on the anatomical and physiological immaturity of the lungs of a premature baby in combination with barotrauma and toxic effects of oxygen during mechanical ventilation. Factors such as concomitant lung diseases (e.g., hyaline membrane disease), congenital heart defects, infections, pulmonary edema (including due to excessive infusion therapy), pulmonary hypertension, genetic predisposition and hypovitaminosis A and E. also play a role.
The immature lungs of a premature baby are characterized by a deficiency of surfactant , a natural surfactant that prevents the alveoli from falling off on exhalation and is necessary for the implementation of bactericidal mechanical evacuation of mucus by the ciliary epithelium. Surfactant begins to be synthesized at 20-24 weeks of gestation, the required level of production is reached by 35-36 weeks. A particularly intense release of surfactant occurs during childbirth. In premature infants, there is both insufficient synthesis and insufficient release of surfactant. Moreover, the synthesis deficit is associated not only with birth in the early stages of gestation, but also with the inhibition of surfactant synthesis due to concomitant pathology (hypoxia, infection).
BPD has an iatrogenic element - mechanical ventilation, especially in harsh conditions, is associated with barotrauma of the bronchiolar and lung tissues, while the toxic effect of high oxygen concentrations of the inhaled mixture also leads to damage to the epithelium, the development of pulmonary edema and its impregnation with protein. As a result, both factors lead to a decrease in the extensibility of the alveoli, which, according to the mechanism of the vicious circle, exacerbates barotrauma.
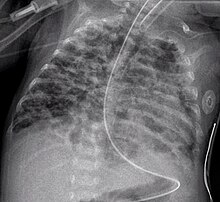
By W. Norsway et al. (1967), there are 4 stages of BPD formation, according to the results of pathological studies: the first stage (1-3 days of life) - pronounced alveolar and interstitial edema with hyaline membranes, atelectasis and necrosis of the bronchiole endothelium; the second stage (4-10th days of life) - atelectases become more common and alternate with areas of emphysema, areas of necrosis and repair of the epithelium of the bronchioles spread, necrotic masses fill the airways, and on the chest radiograph is an “air bronchogram” , pulmonary fields are darkened in some places, but areas of interstitial emphysema are also obvious; the third stage (11 — ZO-th days of life) - common metaplasia and hyperplasia of the epithelium of the bronchi and bronchioles, areas of emphysema surrounded by zones of atelectasis, massive interstitial fibrosis and edema with thinning of the basement membranes, alveoli, on the radiograph - areas of inflammation, atelectasis zones and the appearance of cysts; the fourth stage (second month of life) - massive pulmonary fibrosis with destruction of the alveoli and airway walls (with metaplasia of the epithelium), hypertrophy of the muscle layer of bronchioles, a decrease in the number of pulmonary arterioles and capillaries with hypertrophy of the muscle layer of arterioles and venules, radiological - Ki - massive pulmonary fibrosis with edema and areas of inflammation, seals. So, the morphological basis of BPD is the development of interstitial and intraalveolar fibrosis against the background of immature lung anatomical structures. Sites of interstitial fibrosis are detected in sections in children who die from SDR, combined with grade III – IV high fatty acids, already at the end of the first and the beginning of the second week of life (Dementieva G.M. et al., 2000; Popov S.D., 2002). In the future, fibrous changes in the lungs become more common, with histological examination (in patients who died from SDR), extensive fields of atelectases are found, degenerative changes in the alveolocytes and bronchial epithelium, hyperplasia and metaplasia of the bronchial epithelium in a multilayer flat with small patches of emphysema. The interalveolar septa are thickened, swollen; fibroblast elements proliferate in interstitium with hyperproduction of fibrous structures. In some parts of the lungs, a complete obliteration of the lumen of the respiratory department of the lungs (bronchioles, alveolar passages, alveoli) is noted. Often hyaline membranes are also revealed in sections. In the pathogenesis of these lesions, crucial importance is given to: • immaturity of the lung tissue; • excessive formation of peroxide compounds; • insufficient activity of the antioxidant defense system, which contributes to destructive processes in the lungs; • pulmonary edema in the first days of life contributes to these processes. On the ECG and Echocardiography, as BPD progresses, right ventricular hypertrophy, increased pulmonary vascular resistance, and then left ventricular hypertrophy are naturally noted. Thus, BPD is a chronic inflammatory process in the lungs of mixed origin. Markers of chronic inflammatory response in BPD. In bronchoalveolar lavage in children with BPD, there is an increased content of neutrophils with an increased lifespan, increased activity of elastase, fibronectin, as well as inflammatory mediators such as leukotrienes, platelet activation factor. In the daily urine of these children, the release of desmosin is increased in the first week of life, indicating an increased degradation of lung elastase. Increased production of elastase, which destroys the elastin of the alveolar wall, can lead to impaired formation and growth of the lung, hyperreactivity of the bronchi and pulmonary vessels. An increased concentration of pro-inflammatory cytokines (IL1, IL6, IL8, TNFa) contributes to bronchoconstriction and vasoconstriction of pulmonary arterioles, characteristic of children with BPD, and increased permeability of the alveolar capillary walls. The crucial role in the formation and maintenance of a chronic inflammatory process in the lungs with BPD, in our opinion, is played by activated maternal lymphocytes that reach the child and cause cellular hyperplasia of the connective tissue of his lungs against the background of a peculiar hormonal background. BPD is a variant of chronic obstructive pulmonary disease (COPD). Obstructive syndrome in children with BPD can be caused both by persistent morphological changes in the airway wall, hyperplasia of the muscle layer of the bronchioles wall, obstructive bronchiolitis, and also be functional, associated with hyperreactivity - bronchospasm in cold air, physical activity, infection , and possibly aerosol antigens. In different patients with BPD, the specific gravity of these components in the genesis of obstructive syndrome, of course, is different.
Clinic
The initial stages of BPD are characterized by the fact that usually in a premature baby when conducting mechanical ventilation for SDR, after a week it is not possible to “get away” from the rigid parameters of mechanical ventilation, “dependence” on high values of FiO2. When trying to reduce inspiratory pressure (PIP) or lower the oxygen concentration during respiratory oxygen-air mixture (Fio2) develops respiratory failure with hypoxemia and hypercapnia. The need for high PIP is due to damage and destruction of the airways, a decrease in pulmonary extensibility due to fibrosis and loss of elastic fibers. Dependence on high Fio2 is associated with death, a decrease in the number of pulmonary capillaries and arterioles, impaired capillary-alveolar gas metabolism with interstitial fibrosis, and pulmonary edema. The chest of a child acquires a barrel-shaped form, is swollen, its anteroposterior size is increased (with type I SDR, it looks like a “match box”), there is an intercostal space retraction during breathing. Shortness of breath with difficulty exhaling, wheezing on exhalation is noted; maybe a stridor. However, apnea attacks with bradycardia are also typical for children with BPD. The skin is usually pale with a cyanotic hue. Blood Po2 values in these children in the first half of life remain reduced, often reaching 45-50 torr (mmHg). Noteworthy is the resistance of the X-ray picture of the lungs in the form of alternating sections of low transparency of the lung tissue, more often the medial medial divisions, rough interstitial pattern (fibrosis), and areas of hyperair. In many children, lobar or segmental atelectases are periodically repeated, and some children with severe BPD develop tracheobronchomalacia. When studying the functional state of the lungs, it is revealed: an increase in respiratory rate, a decrease in tidal volume (with relatively normal minute pulmonary ventilation), a low dynamic pulmonary compliance (lung extensibility), an increase in residual volume, signs of increased resistance in bronchioles, a high blood rate, rise of arterioalveolar difference Raco2, hypoxemia. All this leads to an increase in the work of respiration and requires an increase in the calorie content of food. In children with BPD, the acquired infectious processes in the lungs and pneumonia are very frequent, caused not only by bacteria, but also by fungi. They always have severe respiratory viral infections and are especially severely caused by a syncytial virus. Persistent pulmonary hypertension is a characteristic manifestation of BPD; it can lead to right ventricular failure, pulmonary heart disease with cardiomegaly, hepatomegaly, and fluid retention. Usually, children with BDD are prone to regurgitation, vomiting, aspiration of food masses, they are not added enough to the mass, they develop hypotrophy such as a hypostature. In all children with BPD in the first year of life, repeated attacks of bronchial obstructive syndrome are noted, the frequency of anemia, rickets is high, and approximately 15% of children aged 3-4 years have attacks of bronchial asthma (Dementieva G.M. et al., 2000 )
Diagnosis. There are no generally accepted criteria for the early diagnosis of BPD. The following four criteria for the diagnosis of BPD are proposed: • the need for mechanical ventilation for at least 6 days (in our opinion, for three days) in the first week of life (usually with positive expiratory pressure and a long high F102); • Rao2 in the blood is 50 torr (mmHg) or less, and to raise it, oxygen therapy is required up to the age of more than 28 days. (according to Jobe A.N. and Bancalari EH, 2001, up to 36 weeks. gestational age); • chronic respiratory distress (shortness of breath, chest retraction, respiratory sounds detected by auscultation or heard at a distance) and the presence of signs of obvious respiratory failure and signs of periodic bronchial obstructive syndrome lasting at least 28 days; • torpid radiological changes - in the pulmonary fields, dense foci (zones of fibrosis) alternate with zones of increased transparency, ie hyperinflation (“honeycomb”), diaphragm lowered, intercostal spaces widened, heart shadow enlarged, heart contours unclear, blurry. According to AHJobe and E.N. Bancalari (2001), there are three degrees of severity of BPD: Light - the need for oxygen support until the 28th day of life and older, but its cessation is up to 36 weeks. gestational age. Moderate ~ need for oxygen support until the 28th day of life and older, but Fio2 <0.3 at 36 weeks. gestational age. Severe - the need for oxygen support in 36 weeks. gestational age with F1O2> 0.3.
Treatment
BPD treatment is symptomatic and includes oxygen therapy, diet therapy, regimen, pharmacotherapy: the use of bronchodilators, diuretics, glucocorticosteroids, antioxidants.
BPD treatment often requires mechanical ventilation and / or oxygen supply for weeks or months. The pressure in the ventilator and the oxygen concentration in the supplied air must be minimized as much as possible. However, the development of hypoxemia cannot be allowed, since low paO2 contributes to spasm of the vessels of the lungs and can lead to pulmonary hypertension, the development of pulmonary heart and right ventricular failure. It is possible to maintain PaCO2 at a level of 45-60 mm Hg, at a pH of more than 7.25, oxygen saturation - 90-95%, PO2 - 55-70 mm Hg. Art. In torpid hypoxemia, which requires high pressure on the exhale, high-frequency oscillatory ventilation courses are used, which reduces the duration of ventilation, barotrauma and the frequency of BPD.
Mandatory is the monitoring of blood oxygenation and oxygen concentration in the inhaled mixture. Preference is given to continuous transcutaneous monitoring of PO2 or indicators of blood oxygen saturation. After the cessation of mechanical ventilation, oxygen is subsidized in a concentration that allows PO2 to be maintained at 55 mm RT. Art. When these parameters are stable in a child who is in an oxygen tent with an oxygen content of less than 30%, you can switch to the supply of oxygen through a nasal catheter. Hospitalization can be shortened by introducing a home oxygen therapy program. To this end, oxygen concentrators are used.
In connection with increased metabolic needs in case of respiratory failure, ensuring adequate caloric intake of 120-140 kcal / kg / day is of fundamental importance. Depending on the condition of the newborn, nutrition can be carried out parenterally (with the introduction of amino acids at the rate of protein 2-3 g / kg / day and fat emulsions at the rate of 0.5-3 g / kg / day) or using a nasogastric tube. Early administration of colloidal solutions in parenteral nutrition (up to 5–6 days of life) increases the risk of BPD. The daily amount of fluid is limited to the minimum requirements - 100-120 ml / kg / day due to the risk of developing pulmonary edema, especially with persistent ductus arteriosus.
It is necessary to ensure the maximum possible peace and optimal temperature, maintaining the skin temperature at 36.5 ° C. The pharmacological effect of BPD is due to the presence of persistent pulmonary edema, bronchial hyperreactivity, an inflammatory process in the respiratory tract, the constant action of damaging factors, and the course of repair processes in these patients. In children with BPD in the neonatal period, a positive effect is noted after inhalation of salbutamol and berodual. To improve the drainage function of the bronchi, a vibration and percussion massage of the chest is performed. Timely removal of sputum from the endotracheal tube is important. To improve mucociliary clearance, mucolytic drugs are used: acetylcysteine, ambroxol, enteral or inhaled through a nebulizer.
Диуретики применяют у детей с БЛД для улучшения легочной эластичности и уменьшения резистентности дыхательных путей за счет выведения излишков натрия и воды, при этом уменьшается потребность в дополнительном проведении кислородотерапии, хотя её продолжительность может не уменьшаться. Фуросемид (1 мг/кг в/в или в/м или 2 мг/кг внутрь) от 1 до 3 раз в день применяется короткое время (до 1 недели), так как длительное его использование вызывает гиперкальциурию и как следствие - остеопороз, переломы, нефрокальциноз.
Для длительной диуретической терапии (до 2-2,5 месяцев) наиболее подходит сочетание гипотиазида (хлортиазида) по 2 мг/кг/сут и спиронолактона (верошпирона) 2 мг/кг/сут внутрь в два приема. Эти препараты вызывают менее выраженные электролитные нарушения. С 1980-х годов для лечения БЛД стали применять дексаметазон. Существует несколько объяснений эффектов стероидов, ведущих к улучшению функции легких: поддержание бета-адренергической активности, стимуляция продукции антиоксидантов, стабилизация клеточных и лизосомальных мембран, торможение агрегации гранулоцитов и улучшение легочной микроциркуляции, угнетение синтеза простагландинов и лейкотриенов, выведение из легких избытка жидкости, супрессия цитокиновой индукции воспалительной реакции в легочной ткани.
Побочные эффекты при назначении стероидов многочисленны. К ранним осложнениям относят повышение частоты нозокомиальных инфекций, в том числе кандидозов, перфораций и кровотечений желудочно-кишечного тракта, артериальной гипертензии, гипергликемии, гипертрофической кардиомиопатии, отмечаются также задержка роста, транзиторная супрессия функции надпочечников. Отдаленные осложнения включают снижение объема серого вещества головного мозга на 35%, повышение частоты детского церебрального паралича и ухудшение психомоторного развития, слепоты. В связи с этим использование декстаметазона для лечения детей с очень низкой массой тела сократилось.
На основании результатов исследований о последствиях применения дексаметазона у детей с БЛД Американская академия педиатрии приводит следующие рекомендации: 1. Рутинное использование парентерального дексаметазона для профилактики и лечения БЛД у детей с очень низкой массой тела (<1500 г) не рекомендуется. 2. Вне рандомизированных контролируемых исследований применение кортикостероидов должно быть исключительно ситуационным, т.е. у детей, требующих максимальной вентиляционной и кислородной поддержки.
При развившейся БЛД или убедительных клинико-лабораторных данных о высоком риске БЛД особенно у детей с гестационным возрастом менее 30 недель, на 7-10 день жизни обычно назначают дексаметазон. Обычно используется следующая схема: 0,5 мг/кг/сут (2 внутривенных введения или пероральных приема), длительность курса 7 дней. Альтернативой системного применения дексаметазона при БЛД являются будесонид (пульмикорт, бенакорт) и другие ингаляционные стероиды (флутиказон, беклометазон). Суточная доза ингаляционных стероидов составляет примерно 400 мкг/кг, дается в две ингаляции через спейсер (аэрочамбер) или небулайзер. Предварительный анализ результатов многоцентровых испытаний показал, что начатая в первые 3 дня жизни профилактическая терапия будесонидом у недоношенных детей менее 32 недель гестации с тяжелым СДР приводит к достоверному снижению частоты БЛД и укорочению длительности ИВЛ. Обычный курс терапии - 3 дня, но у ряда детей его продлевали до 15 дней (Шабалов Н. П., 2000).
Учитывая важную патогенетическую роль инфекционного воспаления в развитии БЛД, при наличии внутриутробной инфекции, трахеобронхита, пневмонии назначается антибактериальная терапия. Выбор антибиотика производится с учетом предполагаемого возбудителя: цефалоспорины III поколения, имипенемы, аминогликозиды назначаются при частом внутрибольничном инфицировании аэробными грамотрицательными бактериями; макролиды - при атипичной этиологии инфекции.
В настоящее время все парентеральные препараты витамина Е исключены из общей практики из-за неудачных результатов применения, вероятно в связи с мембраностабилизирующим действием, а введение витамина Е внутрь ассоциируется с повышением частоты некротизирующего язвенного колита, что может быть связано с высокой осмолярностью препарата. Нет доказательств того, что витамин Е влияет на частоту или тяжесть БЛД. Вместе с тем, в некоторых отделениях новорожденным с массой тела менее 1 кг или 1,5 кг сразу после рождения однократно внутримышечно вводят 20 мг/кг препарата. Это меньше, чем доза, использовавшаяся в большинстве исследований. Изучение эффективности применения витамина А у детей с БЛД также не дало убедительных результатов.
В связи с тем, что наиболее тяжелое состояние у больных с БЛД отмечается при присоединении вирусной инфекции, рекомендуется соблюдение строго охранительного режима для ребенка. При развитии симптомов ОРВИ назначаются препараты интерферонов (виферон).
Прогноз.
После неонатального периода течение БЛД вол¬нообразно и зависит от выраженности морфологических и функцио¬нальных нарушений. У большинства больных отмечается медленное, но четкое улучшение и нормализация состояния через 6-12 месяцев. Но у части больных нарушения сохраняются длительно, бронхообструктивный синдром усиливается при интеркуррентной респиратор-ной, чаще вирусной, инфекции. БЛД - одна из причин рецидиви¬рующего бронхообструктивного синдрома у детей.
Дети с БЛД до 7-10 лет склонны к более частому возникновению заболеваний, протекающих с обструкцией дыхательных путей. Тяжелые формы БЛД длятся месяцами и приводят или к гибе¬ли больного (в 20% случаев), или к поздно наступающему клиниче¬скому улучшению с сохранением значительных рентгенологических из-менений.
По наблюдениям Г.М.Дементьевой (1997 г.) у 16-20% детей, выписанных из отделений для недоношенных с диагнозом «бронхолегочная дисплазия», сохраняются патологические изменения в легких и в более старшем возрасте - на 1-4 годах жизни, а у 4% больных бронхолегочная дисплазия в дальнейшем приводит к инвалидности.
Реабилитация
Prevention
- Первичная профилактика
Профилактика невынашивания, уменьшение продолжительности ИВЛ и снижение концентрации кислорода во вдыхаемой смеси у недоношенных, находящихся на ИВЛ.
- Вторичная профилактика
БЛД является фактором риска тяжёлого течения респираторно-синцитиальной (РС) инфекции. Для профилактики тяжёлой РС-инфекции в США , Евросоюзе и других странах (всего более 60) применяется паливизумаб , моноклональное гуманизированное антитело против РС-вируса , в России препарат Синагис. Так как препарат дорогостоящий, дети с диагнозом БЛД имеют право на инъекции по квотам.
Forecast
БЛД может приводить или способствовать развитию таких заболеваний дыхательной системы, как рецидивирующий бронхообструктивный синдром (РБОС), острые бронхиолиты, особенно связанные с респираторно-синцитиальной вирусной инфекцией , хроническая дыхательная недостаточность , ателектазы, синдром хронической микроаспирации , пневмония . Описаны сочетания БЛД с синдромом крупа , врождёнными пороками развития лёгких, трансформация в хронический бронхиолит с облитерацией (ХбсО), бронхиальную астму , рецидивирующий обструктивный бронхит(ROB). In children with BPD, eating disorders are common, often associated with prolonged intubation. In such children, oral-tactile hypersensitivity (also known as oral aversion ) is often observed . [one]
Notes
- ↑ Gaining & Growing. Bronchopulmonary dysplasia , Gaining & Growing , March 20 , 2007 . (Retrieved June 12 , 2008. )