Hypothyroidism (from hypo- and lat. (Glandula) thyreoidea - the thyroid gland ) is a condition caused by a prolonged, persistent lack of thyroid hormones , the opposite of thyrotoxicosis . The extreme manifestation of the clinical symptoms of hypothyroidism in adults is myxedema , in children - cretinism .
| Hypothyroidism | |
|---|---|
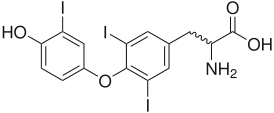 Triiodothyronine , the most active form of thyroid hormones | |
| ICD-10 | E 03.9 |
| ICD-10-KM | |
| ICD-9 | 244.9 |
| ICD-9-KM | |
| Diseasesdb | 6558 |
| Medlineplus | |
| eMedicine | med / 1145 |
| Mesh | D007037 |
Content
General information
Hypothyroidism is a syndrome, a specific condition of the body associated with a reaction to a low concentration of thyroid hormones . When compensating for the necessary level of hormones, these symptoms usually disappear. Hypothyroidism can be associated with functional insufficiency of thyroid hormones or with pathological processes that affect hormonal metabolism. For the first time hypothyroidism as a disease was described in 1873 , and the term “myxedema” (mucous edema of the skin) in relation to severe forms of hypothyroidism began to be used since 1878 .
Etiology
- Primary hypothyroidism is caused by the action of the following factors
- Hypo- or aplasia of the thyroid gland;
- Congenital violation of the synthesis of thyroid hormones;
- thyroiditis;
- Features of nutrition (iodine deficiency, excess of thiocyanates present in cabbage, swede, turnip, turnip, cassava, excess of calcium and lithium ions blocking the capture of iodine);
- Medical actions (removal of the gland, radiation therapy, taking medications).
2. Secondary hypothyroidism (pituitary and hypothalamic)
- Associated with hypopituitarism;
- A defect in the synthesis and transport of thyroliberin from the hypothalamus to the pituitary gland.
3. Tertiary (post-iron)
- It is associated with the inactivation of T3 and T4 circulating in the blood, TSH autoantibodies , proteases in sepsis, pancreatitis , shock;
- It is associated with low sensitivity of target cell receptors to hormones;
- A possible cause is the deiodination of hormones in the peripheral blood.
Pathogenesis
The main cause of spontaneous hypothyroidism is autoimmune thyroiditis and Epstein-Barr virus . The disease often affects older people, mostly women [3] [4] [5] .
The pathogenesis is different, depending on the nature of the lesion:
- Primary hypothyroidism is associated with pathology of the thyroid gland, leading to a decrease in the mass of glandular tissue of the thyroid gland and inhibition of the synthesis of hormones thyroxine and triiodothyronine [6] . This may be a consequence of aplasia or agenesis of the thyroid gland, autoimmune processes , iodine deficiency , selenium deficiency ;
- Secondary hypothyroidism (“central”) is associated with a loss of the tropic function of the pituitary gland (a decrease in thyrotropin production). Insufficient intake of thyroid hormones in the body leads to disruption of protein, carbohydrate metabolism, flattening of the sugar curve after glucose loading, and disruption of lipid , water-salt metabolism [7] .
Epidemiology
Hypothyroidism in Russia occurs with a frequency of 19 per 1000 in women and 21 per 1000 in men. Despite its prevalence, hypothyroidism is very often detected late.
This is due to the fact that the symptoms of the disorder have a gradual onset and erased non-specific forms. Many doctors regard them as a result of overwork or a consequence of other diseases or pregnancy, and do not refer the patient to an analysis of the level of thyroid - stimulating hormones in the blood. Thyroid hormones regulate energy metabolism in the body, so all metabolic processes in hypothyroidism slow down somewhat.
Classification
The following types of hypothyroidism are distinguished:
- Primary (thyrogenic);
- Secondary (pituitary);
- Tertiary (hypothalamic);
- Tissue (transport, peripheral).
As well as:
- Congenital hypothyroidism ;
- Acquired hypothyroidism, including postoperative (after thyroid resection).
According to severity, primary hypothyroidism is divided into:
- Latent (subclinical) - increased TSH level at normal T 4 ;
- Manifest - TSH hypersecretion, with a reduced level of T 4 , clinical manifestations;
- Compensated;
- Decompensated;
- Severe course (complicated). There are serious complications: cretinism , heart failure , effusion in the serous cavities, secondary pituitary adenoma . As a rule, these are unrecognized, neglected cases in time, which without a timely prescribed and correctly selected substitution drug therapy can lead to the development of hypothyroid, or myxedema coma .
Clinical manifestations
Complaints are often scarce and nonspecific, the severity of the patient’s condition usually does not correspond to their complaints: lethargy, slowness, decreased working capacity and fatigue, drowsiness, memory loss, many often complain of dry skin, puffiness of the face and swelling of the limbs, rough voice, brittle nails, loss of hair hair, an increase in body weight with a decrease in appetite, [8] a feeling of chilliness, paresthesia, constipation, and other symptoms are noted. The severity of the symptoms of hypothyroidism largely depends on the cause of the disease, the degree of thyroid failure, the individual characteristics of the patient.
Hypothyroidism-Specific Syndromes
Hypothermic metabolic syndrome: obesity, lowering temperature, coldness, cold intolerance, hypercarotinemia, causing yellowness of the skin.
Myxedema edema: periorbital edema, puffy face, large lips and tongue with imprints of teeth along the lateral edges, edematous limbs, difficulty in nasal breathing (due to swelling of the nasal mucosa), hearing impairment (edema of the auditory tube and middle ear organs), hoarse voice ( swelling and thickening of the vocal cords), polyserositis.
Nervous system damage syndrome: drowsiness, lethargy, decreased memory, attention, intelligence, bradyphrenia, muscle pain, paresthesia, decreased tendon reflexes, polyneuropathy, depression, cerebellar ataxia . Untreated hypothyroidism in newborns leads to mental and physical retardation (rarely reversible), cretinism .
Cardiovascular disease: myxedema heart ( bradycardia , low voltage, negative T wave with ECG, circulatory failure), hypotension, polyserositis, atypical options are possible (with hypertension, without bradycardia, with constant tachycardia with circulatory failure and paroxysmal tachycardia type of sympathetic-adrenal crises in the debut of hypothyroidism).
Excretory system lesion syndrome: decreased filtration and absorption .
Impairment of the musculoskeletal system: joint swelling, pain during movement, generalized skeletal muscle hypertrophy, moderate muscle weakness, Hoffman syndrome.
Digestive system syndrome: hepatomegaly, biliary duct dyskinesia, colon dyskinesia, tendency to constipation, decreased appetite, atrophy of the gastric mucosa, nausea, and sometimes vomiting.
Anemic syndrome: anemia - normochromic normocytic, hypochromic iron deficiency, macrocytic, B12-deficient.
Hyperprolactinemic hypogonadism syndrome: ovarian dysfunction (menorrhagia, oligomenorrhea or amenorrhea, infertility), galactorrhea in women, in men - decreased libido, erectile dysfunction .
Syndrome of ectodermal disorders: changes in the hair, nails, skin. Hair is dull, brittle, falls out on the head, eyebrows, limbs, and slowly grows. Dry skin. The nails are thin, with longitudinal or transverse striation, exfoliate.
Hypothyroid ( myxedema ) coma.
This is the most severe, sometimes fatal complication of hypothyroidism. It is characterized by a progressive increase in all of the above symptoms of hypothyroidism. Mortality reaches 40%. This complication occurs most often in older women with long-term undiagnosed or untreated (poorly treated) hypothyroidism. Provoking factors are usually hypothermia and lack of exercise, cardiovascular failure, acute infectious diseases, psycho-emotional and physical overload, taking sleeping pills and sedatives, and alcohol.
Pediatric hypothyroidism
Symptoms: prolonged physiological jaundice, large tongue, narrow palpebral fissures, constipation, bradycardia , hypothermia , mucinous or mucous edema, late closure of the large fontanel and teething, poor increase in body weight and growth, delayed psychophysical development.
To establish a diagnosis of hypothyroidism, it is enough to determine the total T4, free T4 and TSH in serum.
Diagnostics
Differential diagnosis is based on clinical studies of the patient, in particular, levels of thyroid hormones for some time. Thyroxine (T4-norm - 50-140 nmol / L for children older than 2 months) and triiodothyronine (T3-norm - 1.50-3.85 mmol / L) are determined. With hypothyroidism, their level decreases in proportion to the severity of the disease, the level of TSH is sharply increased. Certain changes in the levels of thyroid hormones are possible under the influence of adverse environmental conditions, under the influence of factors of professional activity (chemicals, radiation ).
Differential Diagnostics
The differential diagnosis is carried out with other endocrinopathies: growth retardation and nanism , encephalopathy, chondrodystrophy, rickets , Hirschsprung’s disease .
Treatment
Treatment is based on differential diagnosis. In complex treatment, replacement therapy with cattle thyroid gland drugs or, more often, synthetic thyroid hormones ( thyroidin , triiodothyronine , thyroxine , thyrotome , thyrotome-fort, thyrecomb ) is used. The dose is determined individually in each case.
See also
- Goiter
- Myxedema
- Hyperthyroidism
Notes
- ↑ Disease Ontology release 2019-05-13 - 2019-05-13 - 2019.
- ↑ Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018.
- ↑ Valdina E.A. Thyroid diseases. - SPb. : Peter, 2001 .-- 416 p.
- ↑ Garkunova L.V., Ametov A.S. The state of the cardiovascular system in patients with hypothyroidism in old age // Ter. arch. - 2004. - No. 12. - S. 97-99.
- ↑ Kasyanova N.A., Sviridenko N. Yu. Subclinical hypothyroidism // Attending physician. - 2006. - No. 10. - S. 58–61.
- ↑ Petunina N. Cardiovascular complications of hypothyroidism // Doctor. - 2007. - No. 4. - S. 2-5.
- ↑ Cardiovascular complications of hypothyroidism. - N.F. Shustval, K. honey. n., associate professor; K.N. Yeshchenko, Ph.D. n .; A.V. Zhadan, Ph.D. N., Associate Professor // Diabetes and Heart, No. 10 (146) / 2010. P. 20-27.
- ↑ Hypofunction of the thyroid gland (Russian) (May 5, 2017). Date of treatment November 13, 2018.
Links
- Hypothyroidism / Medline